Sleep Apnea Update: A Personal Trainer for My Tongue by Robin Gorman Newman
Ever since I was little, yet old enough to wear braces, I recall being told I had a tongue thrust.
My tongue was like a rebellious kid refusing to play by the rules. It presented challenges in elementary school when I was assigned the baritone horn and later the flute in music class. I was not able to blow either correctly. Ultimately, I traded them in for the drums, and I would happily bang away on my drum practice pad. I never progressed enough to get an actual set of drums or even one drum.
I’ve never been able to roll my tongue into certain positions inside my mouth, nor can I whistle, and most recently, I discovered I can’t vibrate my lips in the way that most can — I learned this in an attempt to play the Didgeridoo (which I blogged about previously).
What I didn’t know all these years is that having tongue challenges can be a contributing factor in obstructive sleep apnea. That, combined, in my case, with a narrow airway and one where the uvula isn’t visible when you peer into my throat, is a potential recipe for the disorder. With sleep apnea, your tongue falls back in your throat during sleep and blocks your airway causing lack of breathing episodes and depleted oxygen entering your body.

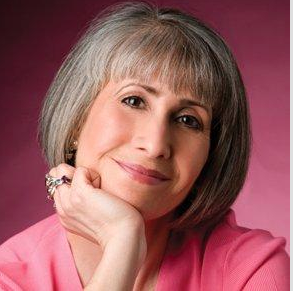
(Ruth Marsillani)
Had I seen a tongue expert early on, I might have gotten “tongue therapy,” and as an adult, I’d potentially have a tongue like a Ninja warrior. Who knew that would be something to aspire to?!
My tongue was recently put to the test when I had an orofacial myofunctional full evaluation with Ruth Marsillani, BA, RDH, Orofacial Myofunctional Therapist and co-founder, Manhattan Myofunctional Therapy LLC in midtown NYC. Ruth is a women on a mission…..she is earnest in her quest to better the lives of her patients and make inroads in this arena. “Sleep apnea, if untreated, can lead to a cocktail of ailments,” and she is a cheerleader for patients who are struggling and those who have yet to seek treatment.
I found her to be kind, supportive, empathetic, highly skilled, well-trained and informed, and the whole experience was quite eye opening (or jaw dropping). It was the first time I had measurements, photos and video taken of my tongue and mouth…so that my before/after experience and progress may be documented. She found that my tongue is large, has a loss of tone, and a natural low rest posture. And, she shared that my having my tonsils taken out as a child could have potentially led to mouth breathing, which is detrimental. (Ruth explained that adenoids and tonsils may cause mouth breathing. She is not against them being removed at a doctor’s recommendation, but advocates that myofunctional therapy is then advisable because the mouth breathing habit may remain.) Additionally, I was a thumb sucker, which affects the shape of the palate (making it narrow and high vaulted…which you don’t want). My lower jaw and chin is retruded back a bit, which impinges on my airway. Plus, I had four teeth pulled as a teen when I got braces because my mouth was overcrowded, and this, too, impacts the size of the jaw. And, it turns out tongue control, or lack thereof, can be genetic.
The insight and findings were a lot to swallow, literally, and made me feel like I’ve been destined for sleep apnea. I became acutely aware of what parents should know with regard to the oral care of their children. We might be able to help future sleep apnea patients ward off the scenario by better understanding the causes which can take root in youth.

(Tongue Tools)
I left her office with a goody bag of “tongue tools,” that my 13 year old son found quite intriguing…from teeny rubberbands, to cork, to balloons to chopsticks. I can only imagine what is in store for me. My initial instructions were to perform three tasks — each twice/daily. They include making a sharp Kah, Kah, Kah sound 25 times, and Ah, Ah, Ah, also 25 times. Each is done while looking in a mirror to make sure my soft palate and tongue are moving. I am also to brush my tongue (with a brush I was given) 10 times, stroking the sides and center. I was told that this, with consistency, has the potential to reduce the size and build the strength of my tongue. “The tongue is a muscle and should be able to work independently,” she says.
None of this is a quick fix or a guaranteed result, and it takes commitment, and every case is different. More exercises will be added as we move along. We will be doing weekly Skype sessions, with periodic in-person 30-40 minute office visits to physically check on my tongue. Ruth shared that one of her patients after a year of following her custom program was able to get off a CPAP mask. This doesn’t happen for everyone. I should be so fortunate, and would be ever grateful. Losing weight is also highly advisable, as fat deposits in the neck and throat area have an impact. Some patients wear an oral appliance in addition to doing the therapy, but you don’t have to. Nutrition can even play a role, for example, Gluten causes inflammation in some people, which can increase the severity of sleep apnea. Hormones and aging, too, for women, are a factor, because you may lose elasticity including of the soft palate.

(Tongue Selfie)
Ruth explained that doing oral facial myofunctional therapy helps create mind-body control. ” You, your tongue and your brain have to agree that you have a connection and that you can build upon that. The goal is to re-pattern the signal from the brain to the muscle, so you can acquire new healthy habits and feel the benefits from the exercise. And, it’s never too late to teach an old dog new tricks,” she said. Ruth, who thinks of herself as a coach to help guide you along, recommends as a potential starting point a book called Close Your Mouth by Patrick McKeown. “It takes a village to raise a child. It takes a village to help a patient with sleep apnea,” she says, and sometimes that also includes referring patients to other practitioners when more needs to be done beyond her work with them. She does not recommend that a patient stop using the CPAP or a dental (Mandibular advancement) device for the treatment of sleep apnea until a sleep study is done and at the advisement of a physician.
More and more research is being pursued in this arena worldwide, and this type of therapy is receiving a heightened level of attention in the medical community. This is highly encouraging for those of us open to trying new techniques. I continue to wear my CPAP nasal mask nightly (though some nights I yearn to yank it off), and am working on weight loss, and I hope that I may one day be free of the mask and return to a new “normal” of sleep. And, if not, at least I will know my tongue and I gave it a valiant effort.
.